10 Questions and Observations That Will Help You Choose a Dentist
Many situations can occur that may require us to find a new dentist such as moving, having a dentist retire, or needing special services our dentist can't provide. Although we all know that proper dental care is vital to good health, most of us don't know how to choose a good dentist. It can be difficult to know what questions to ask and what things to observe in the process of choosing a good dentist. You will want to know both how the dentist treats you as a person and how he treats your mouth. Following are some key questions to ask and observations to make in the process of making your choice.
Full article click here
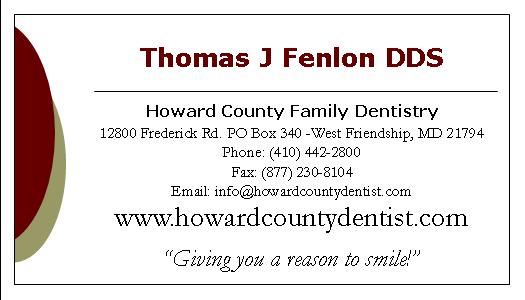
To learn more about this or you have any questions please feel free to visit our website at www.howardcountydentist.com. Call us at (410)-442-2800 or email us at info@howardcountydentist.com
Tuesday, June 16, 2009
Tuesday, June 9, 2009
Snoring May Impair Brain Function
Snoring May Impair Brain Function
It has been linked to learning impairment, stroke and premature death. Now UNSW research has found that snoring associated with sleep apnea may impair brain function more than previously thought.
Sufferers of obstructive sleep apnea experience similar changes in brain biochemistry as people who have had a severe stroke or who are dying, the research shows.
A study by UNSW Brain Sciences, published this month in the Journal of Cerebral Blood Flow and Metabolism, is the first to analyze - in a second-by-second timeframe - what is happening in the brains of sufferers as they sleep. Previous studies have focused on recreating oxygen impairment in awake patients.
"It used to be thought that apnea snoring had absolutely no acute effects on brain function but this is plainly not true," said lead author of the study, New South Global Professor Caroline Rae.
Sleep apnea affects as many as one in four middle-aged men, with around three percent going on to experience a severe form of the condition characterized by extended pauses in breathing, repetitive asphyxia and sleep fragmentation.
Children with enlarged tonsils and adenoids are also affected, raising concerns of long-term cognitive damage.
Professor Rae and collaborators from Sydney University's Woolcock Institute used magnetic resonance spectroscopy to study the brains of 13 men with severe, untreated, obstructive sleep apnea. They found that even a moderate degree of oxygen de-saturation during the patients' sleep had significant effects on the brain's bioenergetics status.
"The findings show that lack of oxygen while asleep may be far more detrimental than when awake, possibly because the normal compensatory mechanisms don't work as well when you are asleep," Professor Rae, who is based at the Prince of Wales Medical Research Institute, said.
"This is happening in someone with sleep apnea acutely and continually when they are asleep. It's a completely different biochemical mechanism from anything we've seen before and is similar to what you see in somebody who has had a very severe stroke or is dying."
The findings suggested societal perceptions of snoring needed to change, Professor Rae said.
"People look at people snoring and think it's funny. That has to stop."
Professor Rae said it was still unclear why the body responded to oxygen depletion in this way. It could be a form of ischemic preconditioning at work, much like in heart attack sufferers whose initial attack makes them more protected from subsequent attacks.
"The brain could be basically resetting its bioenergetics to make itself more resistant to lack of oxygen," Professor Rae said. "It may be a compensatory mechanism to keep you alive, we just don't know, but even if it is it's not likely to be doing you much good."
To learn more about this or you have any questions please feel free to visit our website at www.howardcountydentist.com. Call us at(410)-442-2800 or email us at info@howardcountydentist.com
It has been linked to learning impairment, stroke and premature death. Now UNSW research has found that snoring associated with sleep apnea may impair brain function more than previously thought.
Sufferers of obstructive sleep apnea experience similar changes in brain biochemistry as people who have had a severe stroke or who are dying, the research shows.
A study by UNSW Brain Sciences, published this month in the Journal of Cerebral Blood Flow and Metabolism, is the first to analyze - in a second-by-second timeframe - what is happening in the brains of sufferers as they sleep. Previous studies have focused on recreating oxygen impairment in awake patients.
"It used to be thought that apnea snoring had absolutely no acute effects on brain function but this is plainly not true," said lead author of the study, New South Global Professor Caroline Rae.
Sleep apnea affects as many as one in four middle-aged men, with around three percent going on to experience a severe form of the condition characterized by extended pauses in breathing, repetitive asphyxia and sleep fragmentation.
Children with enlarged tonsils and adenoids are also affected, raising concerns of long-term cognitive damage.
Professor Rae and collaborators from Sydney University's Woolcock Institute used magnetic resonance spectroscopy to study the brains of 13 men with severe, untreated, obstructive sleep apnea. They found that even a moderate degree of oxygen de-saturation during the patients' sleep had significant effects on the brain's bioenergetics status.
"The findings show that lack of oxygen while asleep may be far more detrimental than when awake, possibly because the normal compensatory mechanisms don't work as well when you are asleep," Professor Rae, who is based at the Prince of Wales Medical Research Institute, said.
"This is happening in someone with sleep apnea acutely and continually when they are asleep. It's a completely different biochemical mechanism from anything we've seen before and is similar to what you see in somebody who has had a very severe stroke or is dying."
The findings suggested societal perceptions of snoring needed to change, Professor Rae said.
"People look at people snoring and think it's funny. That has to stop."
Professor Rae said it was still unclear why the body responded to oxygen depletion in this way. It could be a form of ischemic preconditioning at work, much like in heart attack sufferers whose initial attack makes them more protected from subsequent attacks.
"The brain could be basically resetting its bioenergetics to make itself more resistant to lack of oxygen," Professor Rae said. "It may be a compensatory mechanism to keep you alive, we just don't know, but even if it is it's not likely to be doing you much good."
To learn more about this or you have any questions please feel free to visit our website at www.howardcountydentist.com. Call us at(410)-442-2800 or email us at info@howardcountydentist.com
Monday, June 8, 2009
Studies Show that People with Sleep Apnea have a High Risk of Death
A study in the August 1 issue of the journal Sleep shows that people with severe sleep apnea have a much higher mortality risk than people without sleep apnea, and this risk increases when sleep apnea is untreated. Results show that people who have severe sleep apnea, which involves frequent breathing pauses during sleep, have three times the risk of dying due to any cause compared with people who do not have sleep apnea. This risk is represented by an adjusted hazard ratio of 3.2 after controlling for age, sex and body mass index. When 126 participants who reported regular use of continuous positive airway pressure (CPAP) therapy were removed from the statistical analysis, the hazard ratio for all-cause mortality related to severe sleep apnea rose to 4.3.
"We found that both men and women with sleep apnea in the general population - not patients - mostly undiagnosed and untreated, had poorer survival compared with persons without sleep apnea, given equa! l BMI, a ge and sex," said principal investigator and lead author Terry Young, PhD, professor of epidemiology at the University of Wisconsin-Madison.
According to Young, most previous studies of sleep apnea and mortality have involved patients referred for a clinical sleep diagnostic evaluation; the mortality risk for sleep apnea in the general population has not been previously reported.
The study was an 18-year follow-up of 1,522 participants in the ongoing Wisconsin Sleep Cohort Study, which was established in 1988 and involved a random sample of men and women from the community who were between the ages of 30 and 60 when the study began. After spending one night at the University of Wisconsin General Clinical Research Center for assessment by polysomnography, participants were categorized by apnea-hypopnea index (AHI), which is the average number of breathing pauses (apneas) and reductions (hypopneas) per hour of sleep. Sixty-three individuals (about four percent) had severe sleep apnea at baseline with an AHI of 30 or more and a range of 30 to 97 apneas and hypopneas per hour. About 76 percent of the study group (1,157 individuals) had no sleep apnea with an AHI of less than five.
For the follow-up study, state and national death records were reviewed up to 3/1/08, to identify participants who had died and to note the causes of death listed on the death certificates. Eighty deaths were recorded, including 37 deaths attributed to cancer and 25 deaths attributed to cardiovascular disease and stroke.
About 19 percent of participants with severe sleep apnea died (12 deaths), compared with about four percent of participants with no sleep apnea (46 deaths). Although participants with mild sleep apnea (AHI of five to 14) or moderate sleep apnea (AHI of 15 to 29) had a mortality risk that was 50 percent greater than those with no sleep apnea, the results did not achieve statistical significance.
Hazard ratios for all-cause mortality remained high after further adjustments! for oth er factors such as smoking, alcohol use, sleep duration and total cholesterol. Severe sleep apnea was associated with increased mortality whether or not participants experienced daytime sleepiness.
About 42 percent of deaths in people with severe sleep apnea (5 of 12 deaths) were attributed to cardiovascular disease or stroke, compared with 26 percent of deaths in people with no sleep apnea (12 of 46 deaths). When the 126 participants who reported regular CPAP use were removed from the analysis, the hazard ratio for cardiovascular mortality soared from 2.9 to 5.2 for people with severe sleep apnea. The results suggest that regular CPAP use may protect sleep apnea patients against cardiovascular death.
"I was surprised by how much the risks increased when we excluded people who reported treatment with CPAP," Young said. "Our findings suggest - but cannot prove - that people diagnosed with sleep apnea should be treated, and if CPAP is the prescribed treatment, regular use may prevent premature death."
Statistical adjustments show that high blood pressure, cardiovascular disease, stroke and diabetes may play a role in the association between sleep apnea and mortality, but the specific mechanisms by which sleep apnea contributes to mortality remain unclear.
The study was supported by grants from the National Institutes of Health.
According to the American Academy of Sleep Medicine, obstructive sleep apnea (OSA) involves a decrease or complete halt in airflow despite an ongoing effort to breathe. It occurs when the muscles relax during sleep, causing soft tissue in the back of the throat to collapse and block the upper airway.
The most common treatment for OSA is CPAP therapy, which provides a steady stream of air through a mask that is worn during sleep. This airflow keeps the airway open to prevent pauses in breathing and restore normal oxygen levels.
To learn more about this or you have any questions please feel free to visit our website at www.howardcountydentist.com. Call us at(410)-442-2800 or email us at info@howardcountydentist.com
"We found that both men and women with sleep apnea in the general population - not patients - mostly undiagnosed and untreated, had poorer survival compared with persons without sleep apnea, given equa! l BMI, a ge and sex," said principal investigator and lead author Terry Young, PhD, professor of epidemiology at the University of Wisconsin-Madison.
According to Young, most previous studies of sleep apnea and mortality have involved patients referred for a clinical sleep diagnostic evaluation; the mortality risk for sleep apnea in the general population has not been previously reported.
The study was an 18-year follow-up of 1,522 participants in the ongoing Wisconsin Sleep Cohort Study, which was established in 1988 and involved a random sample of men and women from the community who were between the ages of 30 and 60 when the study began. After spending one night at the University of Wisconsin General Clinical Research Center for assessment by polysomnography, participants were categorized by apnea-hypopnea index (AHI), which is the average number of breathing pauses (apneas) and reductions (hypopneas) per hour of sleep. Sixty-three individuals (about four percent) had severe sleep apnea at baseline with an AHI of 30 or more and a range of 30 to 97 apneas and hypopneas per hour. About 76 percent of the study group (1,157 individuals) had no sleep apnea with an AHI of less than five.
For the follow-up study, state and national death records were reviewed up to 3/1/08, to identify participants who had died and to note the causes of death listed on the death certificates. Eighty deaths were recorded, including 37 deaths attributed to cancer and 25 deaths attributed to cardiovascular disease and stroke.
About 19 percent of participants with severe sleep apnea died (12 deaths), compared with about four percent of participants with no sleep apnea (46 deaths). Although participants with mild sleep apnea (AHI of five to 14) or moderate sleep apnea (AHI of 15 to 29) had a mortality risk that was 50 percent greater than those with no sleep apnea, the results did not achieve statistical significance.
Hazard ratios for all-cause mortality remained high after further adjustments! for oth er factors such as smoking, alcohol use, sleep duration and total cholesterol. Severe sleep apnea was associated with increased mortality whether or not participants experienced daytime sleepiness.
About 42 percent of deaths in people with severe sleep apnea (5 of 12 deaths) were attributed to cardiovascular disease or stroke, compared with 26 percent of deaths in people with no sleep apnea (12 of 46 deaths). When the 126 participants who reported regular CPAP use were removed from the analysis, the hazard ratio for cardiovascular mortality soared from 2.9 to 5.2 for people with severe sleep apnea. The results suggest that regular CPAP use may protect sleep apnea patients against cardiovascular death.
"I was surprised by how much the risks increased when we excluded people who reported treatment with CPAP," Young said. "Our findings suggest - but cannot prove - that people diagnosed with sleep apnea should be treated, and if CPAP is the prescribed treatment, regular use may prevent premature death."
Statistical adjustments show that high blood pressure, cardiovascular disease, stroke and diabetes may play a role in the association between sleep apnea and mortality, but the specific mechanisms by which sleep apnea contributes to mortality remain unclear.
The study was supported by grants from the National Institutes of Health.
According to the American Academy of Sleep Medicine, obstructive sleep apnea (OSA) involves a decrease or complete halt in airflow despite an ongoing effort to breathe. It occurs when the muscles relax during sleep, causing soft tissue in the back of the throat to collapse and block the upper airway.
The most common treatment for OSA is CPAP therapy, which provides a steady stream of air through a mask that is worn during sleep. This airflow keeps the airway open to prevent pauses in breathing and restore normal oxygen levels.
To learn more about this or you have any questions please feel free to visit our website at www.howardcountydentist.com. Call us at(410)-442-2800 or email us at info@howardcountydentist.com
Subscribe to:
Posts (Atom)